Diagnosis of non-coeliac gluten sensitivity (NCGS) requires assessment of improvement whilst following a gluten free diet, after coeliac disease and wheat allergy have been excluded.
If a patient reports non-specific symptoms, such as abdominal pain, bloating, diarrhoea, headaches, or fatigue after consuming foods containing gluten, it is important first to exclude coeliac disease and wheat allergy. The diagnosis is confirmed by an improvement or disappearance of symptoms with a gluten-free diet and a renewed deterioration once gluten is reintroduced. The symptoms usually improve within a few days to two weeks. It is important that the patient follows a diet that contains gluten before the diagnostic process begins.
Medical history
Identifying symptoms and signs
First, it is important to determine if the symptoms described by the patient are typical of NCGS and whether they could be related to the consumption of foods containing gluten. Before starting the diagnosis, the patient should follow a normal diet, i.e. one containing gluten, for at least six weeks.
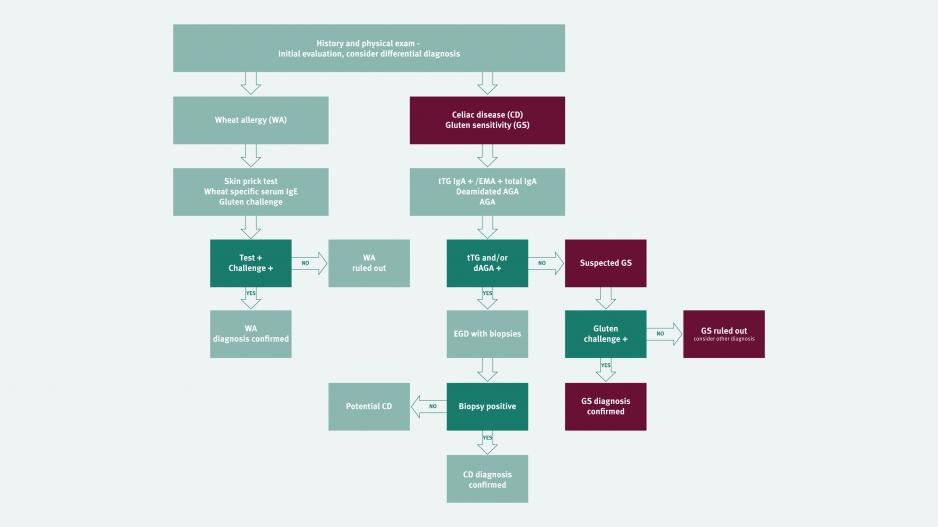
Excluding coeliac disease
Coeliac disease antibody test and biopsy
Since the symptoms of NCGS may resemble those of coeliac disease, it is important to exclude coeliac disease initially. It is crucial to ensure that patients are on a gluten containing diet at the time of investigation. The first step in excluding coeliac disease is coeliac serology (endomysial antibody or tissue transglutaminase antibody). A negative serological test has an excellent negative predictive value in excluding coeliac disease, provided the patient has been consuming a gluten containing diet for 6 weeks prior to the test. In cases with positive serology, a small intestine biopsy is required to confirm a diagnosis of coeliac disease [1]. Patients with NCGS will not have evidence of villous atrophy on duodenal biopsy, although the levels of intra-epithelial lymphocytes (IELs) may be slightly elevated (equating to Marsh scale 1) [2].
Gluten challenge to exclude coeliac disease
If patients are on a gluten free diet at the time of investigation consideration needs to be given to gluten challenge. Current guidelines recommend a 6 week challenge of 10 grams of gluten per day. However many patients with NCGS may not be able to tolerate this amount of gluten and recent evidence suggests that shorter challenges of 2 weeks with 3 grams of gluten are able to confirm coeliac disease in 75% of cases [3]. However duodenal biopsy is required in these cases.
Excluding wheat allergy
IgE-antibody test and skin prick test
The clinical picture of wheat allergy may also be similar to that of NCGS. An IgE antibody test and skin prick test may be used to determine whether a patient is allergic to wheat.
Other evidence of NCGS
IgG anti-gliadin antibody test
IgG anti-gliadin antibodies (AGAs) may be seen more frequently in NCGS [4]. However, AGAs may also be present in people with coeliac disease and in a small proportion of the healthy population. Research is ongoing to clarify the diagnostic procedure for NCGS in the future. At the present time IgG AGA cannot be used for diagnosis.
Gluten-free diet
Improvement in symptoms
If coeliac disease and wheat allergy have been ruled out, the patient may begin a gluten-free diet. In patients with NCGS , symptoms tend to improve or disappear within 14 days. However, it is necessary to follow a gluten-free diet for at least six weeks in order to be able to establish a causal relationship between a gluten-free diet and symptoms. In order to achieve standardisation, the improvement of symptoms should be assessed according to a diagnostic protocol developed at the International Expert Meeting 2014 [5]. This stipulates that the patient identifies 1 - 3 common symptoms and rates their severity on a scale of 1 - 10 before starting a gluten-free diet. This assessment should be carried out two weeks before starting the gluten-free diet and every week thereafter. A good response to the gluten-free diet is indicated by at least 30% improvement in any of the 3 symptoms. At least one symptom should improve, as long as the others do not deteriorate. This improvement should be achieved for a minimum of 50% of the evaluation period, i.e. in at least three of the six weekly reviews.
Re-exposure to gluten
Confirming the diagnosis
As with food allergies, a renewed provocation may be necessary for a definitive diagnosis of NCGS. Following a period of at least 4 weeks on strict gluten free diet, patients should re-introduce gluten. If the symptoms recur within two days patients should restart a gluten free diet followed by a double-blind (for studies) or single-blind (in practice), placebo-controlled oral provocation. The most suitable foods for this purpose are gluten-free bars (as a placebo) and bars containing gluten that do not differ in appearance, texture or flavour. The first one-week trial period is followed by a one-week strict gluten-free diet and a second one-week trial period. The standardised diagnostic protocol should be used for the weekly assessment of symptoms. If a 30% reduction in 1 of the 3 symptom domains is demonstrated in the gluten free period compared to gluten containing period, gluten sensitivity is present.
Diagnostic protocol for gluten/wheat sensitivity
The aforementioned standardised diagnostic protocol was developed by leading researchers in the field of gluten-related disorders at the 3rd International Expert Meeting on Non-Celiac Gluten Sensitivity in October 2014 (5). This stipulates a uniform two-stage dietary process for which a modified version of the gastrointestinal symptom rating scale is used. Patients use this scale to assess the effects of removing and reintroducing gluten on their symptoms. Both gastrointestinal and extraintestinal symptoms are rated on a scale of 1 to 10. This questionnaire is designed to standardise diagnosis.
References
- Mooney, P. D., Hadjivassiliou, M. & Sanders, D. S. Coeliac disease. BMJ 348, g1561 (2014).
- Sapone, A. et al. Divergence of gut permeability and mucosal immune gene expression in two gluten-associated conditions: celiac disease and gluten sensitivity. BMC Med. 9, 23 (2011).
- Leffler DA, Schuppan D, Pallav K et al. Kinetics of the histological, serological and symptomatic responses to gluten challenge in adults with coeliac disease. Gut. 2013 Jul;62(7):996-1004.
- Caio, G., Volta, U., Tovoli, F. & De Giorgio, R. Effect of gluten free diet on immune response to gliadin in patients with non-celiac gluten sensitivity. BMC Gastroenterol. 14, 26 (2014).
- Catassi C, Elli L et al. Diagnosis of Non-Celiac Gluten Sensitivity (NCGS): The Salerno Experts' Criteria. Nutrients. 2015 Jun 18;7(6):4966-77.
