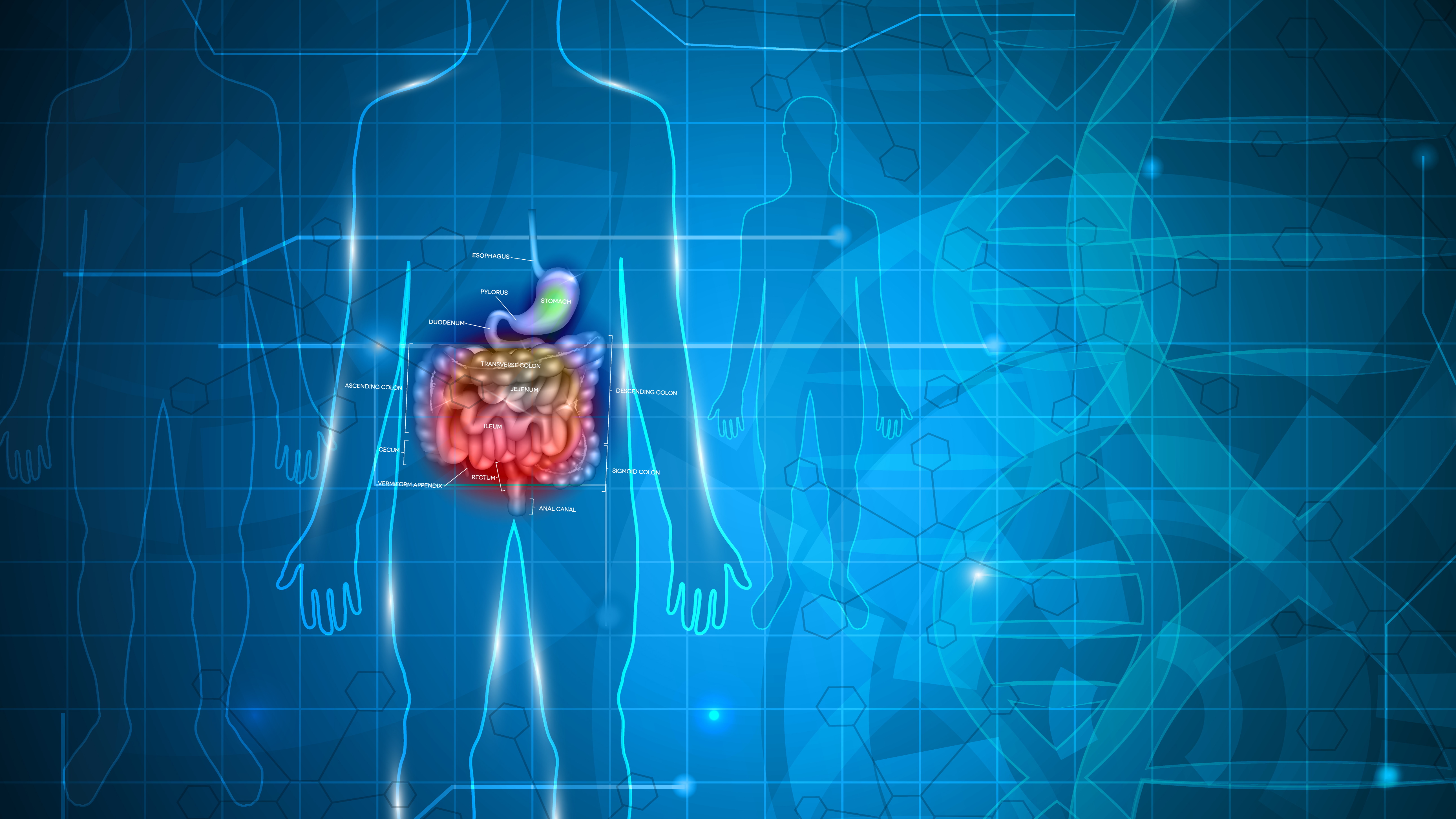
While a balanced diet remains a cornerstone in promoting digestive function, current understanding of the gut-brain axis highlights the important role sleep, exercise, stress and other psychological factors play in maintaining gastrointestinal (GI) homeostasis
The Gut-Brain Axis
The central nervous system (CNS) and the enteric nervous system (ENS) make up the gut-brain axis. Communication between the gut and the CNS is bi-directional via neural, endocrine, and neuroimmune pathways.The vagus nerve, which runs from the brain to the large intestine, facilitates this bi-directional communication between the CNS and ENS. The hypothalamo-pituitary-adrenal (HPA) axis, part of the CNS, coordinates the stress response [1]. The gut-brain axis regulates appetite, digestion and sensory experiences related to digestion. Signals sent from the gut microbiota to the brain alter immune function, intestinal motility, microvascular circulation, nutrient delivery and secretion of digestive enzymes [2].
Disruptions to the gut-brain axis, such as dysbiosis or stress, impair nervous system function and influence changes in mood, stress, anxiety and neurotransmitter production. An overly active ENS that is excessively sensitive to digestive processes accounts for some of the mechanism behind IBS [1]. For example, behavior and thoughts, emanating from the CNS, can influence changes in motility and perception of digestive feelings. Gut microbiota also influence neurotransmitter levels, many of which are produced in the digestive tract, which in turn impact psychological wellbeing [3]. In sum, onset and symptom severity of IBS can be attributed to changes in the nervous system’s reflexive and perceived responses from structural and functional disruption to the gut-brain axis.
Stress, Hormones & Digestion
Stress contributes to IBS pathogenesis as well as symptom severity via the gut-brain axis. The HPA-axis, activated via environmental and systemic stress, secretes corticotropin-releasing factor (CRF), which in turn stimulates the release of adrenocorticotropic hormone (ACTH). ACTH leads to release of cortisol, a major stress hormone that acts on the brain, bones, muscles, body fat and other organs. Cortisol, along with the stress hormone adrenaline, activates the sympathetic nervous system (SNS) and prepares the body to cope with threats [4]. The body responds to all stress with the same response whether it is social, physical or related to poor sleep, real or perceived. When the threat is reduced, levels of stress hormones are reduced.
However, chronic stress leads to chronically elevated levels of cortisol and adrenaline, which has drastic consequences on digestive function. Elevated cortisol and adrenaline inhibit digestion, resulting in reduced production and release of stomach acid and digestive enzymes. Food in turn passes through the digestive tract undigested causing GI symptoms and feeding pathogenic bacteria. Further, cortisol suppresses the immune system and exposes gut associated lymphoid tissue (GALT). This makes the body more vulnerable to bacterial overgrowth and translocation, dysbiosis, chronic inflammation and resulting intestinal permeability. With stress, healing capability is also impaired, reducing the growth and repair rate for intestinal epithelial cells, which already turnover at a high rate. Impaired epithelial cell turnover also contributes to intestinal permeability, making the GI tract even more vulnerable to pathogens [5].
Stress also influences GI homeostasis and digestive function via the vagus nerve. Changes in intestinal motility, visceral hypersensitivity, and inhibition of the migrating motor complex (MMC), the digestive tract’s natural cleansing waves, all result from stress. Patients with visceral hypersensitivity become especially sensitive to digestive feelings, which in itself can contribute to increased stress and anxiety [6]. Gut bacteria also influence mood and anxiety, partly by affecting activity of the vagus nerve [2,7]. The Parasympathetic Nervous System (PSNS) is responsible for saliva, stomach acid, enzyme, and bile production and secretion, nutrient absorption, intestinal motility and the MMC’s cleansing waves. Activation of the PSNS, responsible for activating the body’s “rest and digest” mode, promotes vagus nerve stimulation and proper digestion. This stimulation has a therapeutic effect by promoting relaxation, reducing inflammation and increasing motility, secretion and blood flow to the GI tract [2].
Stress Management for IBS
Stress reduction can both reduce risk for IBS onset, as well as improve symptoms related to dysbiosis, impaired metabolism and intestinal permeability. Clinical guidelines recommend a range of therapeutic interventions for patients with IBS to manage stress and stress-induced responses. A wealth of research supports Cognitive Behavioral Therapy (CBT), as well as gut directed-hypnotherapy, to target cognitive factors that influence symptom experience [8,9,10]. These include how input from the gut is perceived, interpreted, and regulated, such as fear of symptoms, pain catastrophizing, attentional bias, visceral sensitivity, somatization [11]. CBT can also help patients work through trauma and past stressors, which are known to increase risk for IBS [12].
Lifestyle changes, such as meditation, yoga or tai chi, exercise, fresh air and engagement in leisure activities, can also help stimulate the vagus nerve and activate the PSNS [13,14]. Small daily changes to manage stress, such as brief walks during work breaks or using the phone’s “do not disturb” setting a few hours each day, can make a difference in reducing stress. Mindful eating also helps promote PSNS activation and optimal digestion. Prior to starting a meal, recommend that patients sit down, pause and take a few deep breaths. Discourage eating meals while standing up or on-the-go, such as while walking or driving, or while distracted by phones, TV and music. At each meal, help patients to get in the habit of chewing food well, pausing between bites and paying attention to the pleasure and sensory experience of eating. While research is limited, some suggest that cold showers, singing and light massage can also stimulate the vagus nerve.
Diet & Supplements for Symptom Control
Limiting alcohol, caffeine, sugar and processed food helps stabilize energy levels, promote good sleep and manage overall stress. Always encourage patients to prioritize whole foods, complex carbohydrates, fruits and vegetables and eat plenty of healthy fats and lean protein. For some patients, supplements can also play a role in symptom control and stress management.
There is a wealth of evidence to support the use of enteric-coated peppermint oil for IBS. Peppermint oil acts as an antispasmodic and exerts effects on smooth muscle calcium channels and opioid receptors. This contributes to smooth muscle relaxation along the digestive tract, normalized motility and changes in pain sensitivity [15]. Peppermint oil decreases pain, urgency, cramping and bloating related to IBS spasms, though some patients also report increased acid-reflux or heartburn [16]. Generally, one 200 mg tablet of enteric coated peppermint oil (not essential oil) before each meal is an effective dose to alleviate abdominal pain. Chewable simethicone can also be combined with peppermint oil to further reduce gas and bloating.
Though research is limited, there is some preliminary indication targeted and judicious use of supplements may also provide anti-anxiety support. Magnesium is an essential mineral and electrolyte that plays a role in nerve and muscle function, as well as many other bodily functions. The recommended dietary allowance for healthy adults is 310-420 mg/d, though many adults do not meet these needs through diet, and magnesium is not always included in multivitamin formulas [17]. Magnesium supplementation, which is safe up to 1000 mg/day, may have a protective effect against anxiety [18,19]. Magnesium glycinate is highly absorbed and has few GI side effects, while citrate can help address constipation due to its osmotic laxative effect. In addition, though research is highly limited, 1-2 g/d of skullcap flower has also been shown to support stress and anxiety management, while passionflower may provide anti-spasmodic benefits when used intermittently for those with cramping [20,21]. Holy basil is also known to have adaptogenic, antimicrobial, anti-inflammatory, and immunomodulatory properties, which can help manage anxiety, stress and their impact. One hundred and fifty mg of holy basil taken twice per day is generally used, though doses up to 1000 mg/d are considered safe and tolerable [22]. Lastly, lavender oil can also have anti-anxiety effects when used consistently either as an essential oil or when taken as a supplement at a dose of 80 mg/d [23,24,25]. Always use caution when suggesting patients trial supplements and consider potential adverse interactions with other drugs, supplements, or foods. While pills are generally better tolerated, some patients may opt for liquid forms due to brand and formula preferences.
Psychological stress is known to be both a trigger and result of IBS, presenting a bi-directional influence on the gut-brain axis. A focus on stress reduction and management for those with IBS can improve dysbiosis, support food metabolism and absorption by increasing secretions of digestive enzymes, reduce intestinal permeability and promote normalized motility. Lifestyle factors, such as a balanced diet, regular exercise, restful sleep, and relaxation strategies, along with stress management, provide critical support in promoting optimal digestive function
References
- Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 2015;28(2):203-209.
- Breit S, Kupferberg A, Rogler G, Hasler G. Vagus Nerve as Modulator of the Brain-Gut Axis in Psychiatric and Inflammatory Disorders. Front Psychiatry. 2018;9:44. Published 2018 Mar 13. doi:10.3389/fpsyt.2018.00044
- Tang HY, Jiang AJ, Wang XY, et al. Uncovering the pathophysiology of irritable bowel syndrome by exploring the gut-brain axis: a narrative review. Ann Transl Med. 2021;9(14):1187. doi:10.21037/atm-21-2779
- Konturek P, Brzozowski T, Konturek S. Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. J Physiol Pharmacol. 2017;62(6):591-59.
- Liu RT. The microbiome as a novel paradigm in studying stress and mental health. Am Psychol. 2017;72(7), 655-667.http://dx.doi.org/10.1037/amp0000058
- Mönnikes H, Tebbe J, Hildebrandt M, et al. Role of Stress in Functional Gastrointestinal Disorders. Evidence for stress-induced alterations in gastrointestinal motility and sensitivity. Dig Dis. 2001;19(3):201-211. doi:10.1159/000050681.
- Dinan TG, Cryan JF. Gut-brain axis in 2016: Brain-gut-microbiota axis - mood, metabolism and behaviour. Nat Rev Gastroenterol Hepatol. 2017;14(2):69-70. doi:10.1038/nrgastro.2016.200
- Peters SL, Muir JG, Gibson PR. Review article: gut-directed hypnotherapy in the management of irritable bowel syndrome and inflammatory bowel disease. Aliment Pharmacol Ther (2015) 41:1104–15. doi:10.1111/apt.13202
- Laird KT, Tanner-Smith EE, Russell AC, Hollon SD, Walker LS. Comparative efficacy of psychological therapies for improving mental health and daily functioning in irritable bowel syndrome: A systematic review and meta-analysis. Clin Psychol Rev. 2017;51:142-152. doi:10.1016/j.cpr.2016.11.001
- Surdea-Blaga T, Baban A, Nedelcu L, Dumitrascu DL. Psychological Interventions for Irritable Bowel Syndrome. J Gastrointestin Liver Dis. 2016;25(3):359-366. doi:10.15403/jgld.2014.1121.253.ibs
- Lacy BE, Pimentel M, Brenner DM, et al. ACG Clinical Guideline: management of irritable bowel syndrome. Am J Gastroenterol 2021;116:17–44.
- Ng QX, Soh AYS, Loke W, Venkatanarayanan N, Lim DY, Yeo WS. Systematic review with meta-analysis: The association between post-traumatic stress disorder and irritable bowel syndrome. J Gastroenterol Hepatol. 2019;34(1):68-73. doi:10.1111/jgh.14446.
- Brandani, J. Z., Mizuno, J., Ciolac, E. G., & Monteiro, H. L. (2017). The hypotensive effect of yoga’s breathing exercises: A systematic review. Complementary Therapies in Clinical Practice, 28, 38–46.
- Jerath, R., Crawford, M. W., Barnes, V.A., & Harden, K. (2015). Self-regulation of breathing as a primary treatment for anxiety. Applied Psychophysiology and Biofeedback, 40(2), 107–115.
- Patel NV. "Let Food Be Thy Medicine": Diet and Supplements in Irritable Bowel Syndrome. Clin Exp Gastroenterol. 2021;14:377-384. Published 2021 Sep 22. doi:10.2147/CEG.S321054.
- Black CJ, Yuan Y, Selinger CP, et al. Efficacy of soluble fibre, antispasmodic drugs, and gut-brain neuromodulators in irritable bowel syndrome: a systematic review and network meta-analysis. Lancet Gastroenterol Hepatol. 2020;5(2):117-131. doi:10.1016/S2468-1253(19)30324-3.
- Office of dietary supplements - Magnesium. NIH Office of Dietary Supplements. https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/. Accessed December 10, 2022.
- Kirkland AE, Sarlo GL, Holton KF. The Role of Magnesium in Neurological Disorders. Nutrients. 2018;10(6):730. Published 2018 Jun 6. doi:10.3390/nu10060730
- Boyle NB, Lawton C, Dye L. The Effects of Magnesium Supplementation on Subjective Anxiety and Stress-A Systematic Review. Nutrients. 2017;9(5):429. Published 2017 Apr 26. doi:10.3390/nu9050429
- Brock C, Whitehouse J, Tewfik I, Towell T. American Skullcap (Scutellaria lateriflora): a randomised, double-blind placebo-controlled crossover study of its effects on mood in healthy volunteers. Phytother Res. 2014;28(5):692-698. doi:10.1002/ptr.5044
- Kim M, Lim HS, Lee HH, Kim TH. Role Identification of Passiflora Incarnata Linnaeus: A Mini Review. J Menopausal Med. 2017;23(3):156-159. doi:10.6118/jmm.2017.23.3.156.
- Jamshidi N, Cohen MM. The Clinical Efficacy and Safety of Tulsi in Humans: A Systematic Review of the Literature. Evid Based Complement Alternat Med. 2017;2017:9217567. doi:10.1155/2017/9217567
- Malcolm BJ, Tallian K. Essential oil of lavender in anxiety disorders: Ready for prime time?. Ment Health Clin. 2018;7(4):147-155. Published 2018 Mar 26. doi:10.9740/mhc.2017.07.147
- Woelk H, Schläfke S. A multi-center, double-blind, randomised study of the Lavender oil preparation Silexan in comparison to Lorazepam for generalized anxiety disorder. Phytomedicine. 2010;17(2):94-99. doi:10.1016/j.phymed.2009.10.006
- Kasper S, Gastpar M, Müller WE, et al. Lavender oil preparation Silexan is effective in generalized anxiety disorder-a randomized, double-blind comparison to placebo and paroxetine. Int J Neuropsychopharmacol. 2014 Jun;17(6):859-69.
- Bhatia V, Tandon R. Stress and the gastrointestinal tract. J Gastroenterol Hepatol. 2005;20(3):332-339. doi:10.1111/j.1440-1746.2004.03508.x.