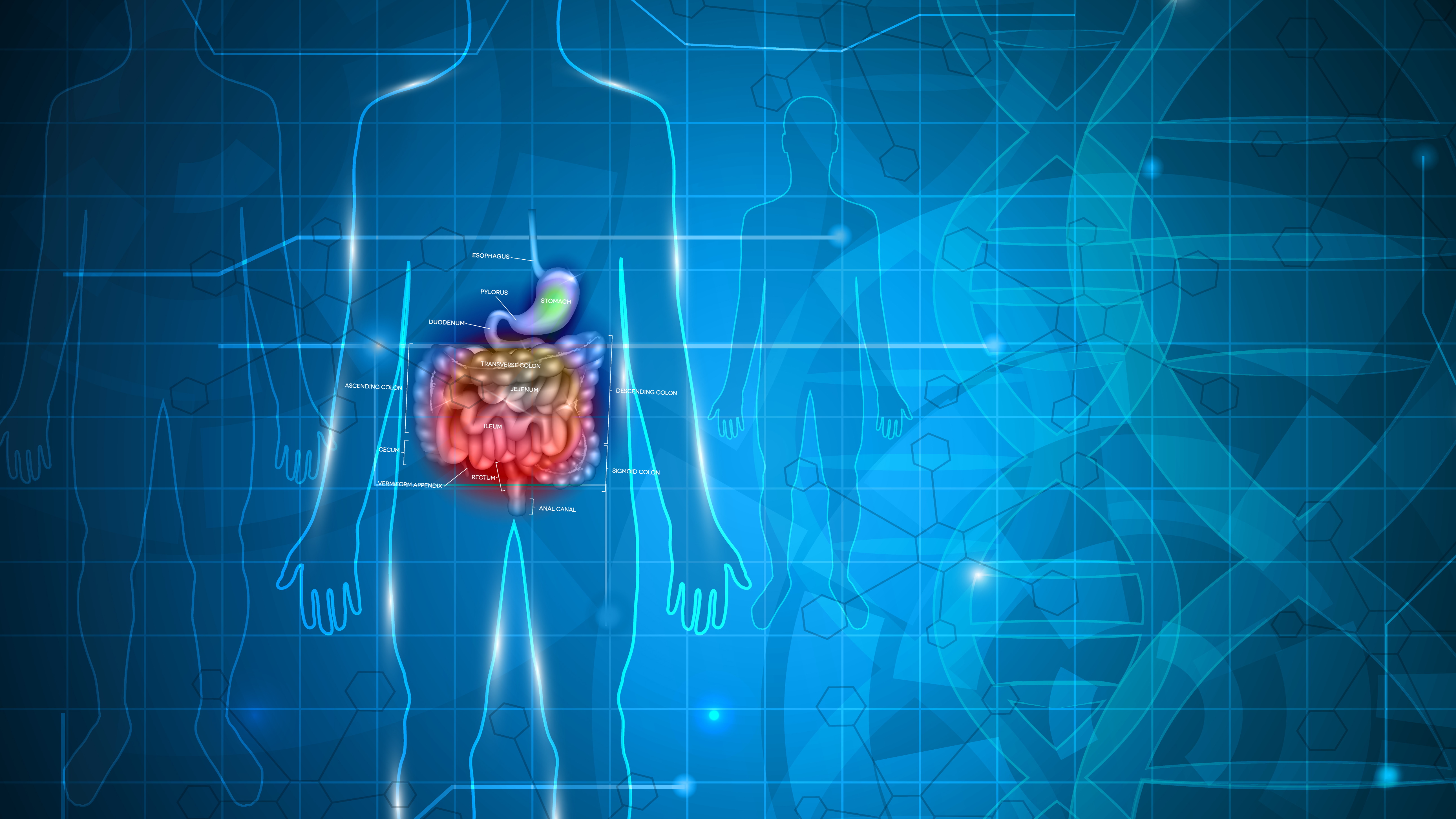
A large focus in the treatment of IBS and other gastrointestinal (GI) conditions is regulation of intestinal permeability and promotion of intestinal barrier function. Both internal factors and external factors contribute to GI integrity. Intestinal epithelial cells serve as the internal system that maintain the balance between the protective immune response against pathogens and the absorption of nutrients. The microbiota, on the other hand, represent the external system, which also helps regulate intestinal permeability [1].
Approaches to repair impaired intestinal permeability, so called “leaky gut,” focus on removal of diet and lifestyle factors that injure GI integrity and promotion of dietary changes and behaviors that support intestinal healing. Since inflammation plays an important role in regulating many necessary immune responses, the goal of treatment is not to remove inflammation entirely. Rather, a targeted approach that reduces and regulates inflammation to fix underlying dysbiosis should be taken.
Supporting Intestinal Barrier Function
Factors that promote a strong immune system also support intestinal health. These include good sleep, stress management and a diverse, nutrient-rich whole foods diet. Work with clients to identify and cut out individual food sensitivities, as they impair GI integrity and increase inflammation. Zonulin is a protein that plays a key role in regulating intestinal permeability and increased levels are associated with loosened tight barriers in the intestinal lining [2]. Zonulin is upregulated by dysbiosis as well as by gluten (specifically gliadin), especially in patients who are sensitive to gluten [3]. Therefore, elimination of individual food sensitivities, pro-inflammatory foods, such as high-sugar, highly-processed foods, and gluten helps reduce the inflammatory immune response.
Limited intake or full elimination of non-steroidal anti-inflammatory drugs NSAIDs and alcohol (if possible) also reduces intestinal injury [4]. As do lifestyle factors that support proper breakdown of foods, such as chewing food well and targeted use of digestive enzymes as clinically indicated.
Addition of nutrients that promote intestinal barrier function is also important. Amino acids support gut integrity by helping heal tight junctions in the intestinal lining [5]. Collagen, unflavored unsweetened gelatin and bone broth are all good sources and generally well-tolerated. One to three grams of omega-3 fatty acids per day, along with antioxidants like Vitamin A, C and E, can also play a role in reducing inflammation [1].
Don’t Forget Fiber
Insoluble and soluble fiber promote development of a healthy intestinal mucous lining and regulating motility. Insoluble fiber, which reaches the colon, is fermented by bacteria to produce short-chain fatty acids (SCFAs), such as butyrate [1,4]. Butyrate is anti-inflammatory and provides important fuel for colon cells and unfortunately often low in patients due to a lack of dietary fiber. Soluble fiber, such as psyllium, is less fermentable and helps manage diarrhea and constipation symptoms by both thickening loose stool and hydrating formed stool without inducing gas or bloating. Excellent food sources of fiber include chia seeds, ground flax, fruits (especially kiwi), vegetables and whole grains. Soluble fiber supplements, such as guar gum (sunfiber) and psyllium husk (Metamucil), are also recommended by ACG clinical guidelines [6]. Notably, some insoluble fibers can exacerbate IBS symptoms so ensure patients are aware of insoluble fiber sources [6].
A Comment on Supplements
A variety of anti-inflammatory supplements may also help repair leaky gut by supporting intestinal barrier function. L-glutamine is a non-essential amino acid that may be used to promote intestinal cell wall integrity, as it feeds intestinal epithelial cells and promotes enterocyte proliferation. Generally needs can be met through a protein-rich diet, though research has shown that supplementation of 15 g/day in tandem with a low-FODMAP diet contributes to a greater reduction in symptom severity than a low-FODMAP diet alone [7]. Research also suggests L-glutamine is effective for patients with post-infectious-IBS [8].
Patients with dysbiosis also commonly have low Vitamin D levels, so acquiring an updated lab value can be very helpful in guiding recommendations. Vitamin D supports the immune system overall, reduces intestinal permeability and promotes healing of the GI lining [9,10]. Autoimmune and inflammatory conditions often impair absorption capacity, so increased doses of Vitamin D may be needed in patients with severe inflammation to adequately restore levels [11]. Doses of 1000-2000IU of D3 depending on seasonality and sun exposure are generally safe and sufficient in patients without pre-existing deficiencies; higher doses may be warranted in those with deficiencies. There is also some evidence that low zinc levels are associated with increased intestinal permeability. These findings have led to a discussion on whether supplementation with zinc carnosine may reduce leaky gut and help regulate the inflammatory immune response [1,12,13]. Note that zinc competes with copper for absorption so supplementation is not recommended long term.
Antioxidants also help regulate the intestinal barrier by fighting free radicals and reducing inflammation. Glutathione is a major antioxidant in the body and supports repair of all cells, including those in the GI tract [14]. Though research is mixed, some suggest N-Acetyl Choline (NAC), which serves as a glutathione precursor, may help treat leaky gut. Antioxidants in the polyphenol category include flavonoids, such as quercetin and curcumin, both of which are phytochemicals found in plants. Quercetin helps stabilize mast cells and has antihistamine properties [1]. Curcumin (from turmeric) has anti-inflammatory and anti-microbial properties that target the trifecta of root causes in IBS and may be particularly effective in those with autoimmune conditions [15,16]. Probiotics may also help promote microbiota homeostasis and reduce specific GI symptoms, though their effectiveness is much debated due to variations in probiotic strains and use-cases studied [1,17].
Remember the pathogenesis of IBS is complex and patient-specific. A holistic approach that considers root causes of dysbiosis, inflammation and intestinal permeability is needed to recommend appropriate and effective therapeutic interventions for each patient’s unique symptom profile.
References
- De Santis S, Cavalcanti E, Mastronardi M, Jirillo E, Chieppa M. Nutritional Keys for Intestinal Barrier Modulation. Front Immunol. 2015;6. doi:10.3389/fimmu.2015.00612
- Lammers KM, Lu R, Brownley J, Lu B, Gerard C, Thomas K, et al. Gliadininduces an increase in intestinal permeability and zonulin release by binding
- Fasano A. All disease begins in the (leaky) gut: role of zonulin-mediated gut permeability in the pathogenesis of some chronic inflammatory diseases. F1000Res. 2020;9:F1000 Faculty Rev-69. Published 2020 Jan 31. doi:10.12688/f1000research.20510.1
- Camilleri M, Lyle BJ, Madsen KL, Sonnenburg J, Verbeke K, Wu GD. Role for diet in normal gut barrier function: developing guidance within the framework of food-labeling regulations. Am J Physiol Gastrointest Liver Physiol. 2019;317(1):G17-G39. doi:10.1152/ajpgi.00063.2019
- Lopetuso LR, Scaldaferri F, Bruno G, Petito V, Franceschi F, Gasbarrini A. The therapeutic management of gut barrier leaking: the emerging role for mucosal barrier protectors. Eur Rev Med Pharmacol Sci. 2015;19(6):1068-1076.
- Lacy BE, Pimentel M, Brenner DM, et al. ACG Clinical Guideline: management of irritable bowel syndrome. Am J Gastroenterol 2021;116:17–44. 16. Black CJ, Yuan Y, Selinger CP, et
- Rastgoo S, Ebrahimi-Daryani N, Agah S, et al. Glutamine Supplementation Enhances the Effects of a Low FODMAP Diet in Irritable Bowel Syndrome Management. Front Nutr. 2021;8:746703. Published 2021 Dec 16. doi:10.3389/fnut.2021.746703
- Zhou Q, Verne ML, Fields JZ, et al. Randomised placebo-controlled trial of dietary glutamine supplements for postinfectious irritable bowel syndrome. Gut. 2019;68(6):996-1002. doi:10.1136/gutjnl-2017-315136
- Sassi F, Tamone C, D’Amelio P. Vitamin D: Nutrient, Hormone, and Immunomodulator. Nutrients. 2018;10(11). doi:10.3390/nu10111656
- Lee C, Lau E, Chusilp S, et al. Protective effects of vitamin D against injury in intestinal epithelium. Pediatr Surg Int. 2019;35(12):1395-1401. doi:10.1007/s00383-019-04586-y
- Williams CE, Williams EA, Corfe BM. Vitamin D status in irritable bowel syndrome and the impact of supplementation on symptoms: what do we know and what do we need to know?. Eur J Clin Nutr. 2018;72(10):1358-1363. doi:10.1038/s41430-017-0064-z
- Mahmood A, FitzGerald AJ, Marchbank T, et al. Zinc carnosine, a health food supplement that stabilises small bowel integrity and stimulates gut repair processes. Gut. 2007;56(2):168-175. doi:10.1136/gut.2006.099929.
- Davison G, Marchbank T, March DS, Thatcher R, Playford RJ. Zinc carnosine works with bovine colostrum in truncating heavy exercise induced increase in gut permeability in healthy volunteers. Am J Clin Nutr. 2016;104(2):526-536. doi:10.3945/ajcn.116.134403.
- Hou Y, Wang L, Yi D, Wu G. N-acetylcysteine and intestinal health: a focus on its mechanism of action. Front Biosci (Landmark Ed). 2015;20:872-891. doi:10.2741/4342.
- Yatoo MI Anti-Inflammatory Drugs and Herbs with Special Emphasis on Herbal Medicines for Countering Inflammatory Diseases and Disorders - A Review. Recent Pat Inflamm Allergy Drug Discov. 2018;12(1):39-58. doi:10.2174/1872213X12666180115153635.
- Maroon JC, Bost JW, Maroon A. Natural anti-inflammatory agents for pain relief. Surg Neurol Int. 2010;1. doi:10.4103/2152-7806.73804.
- Fasano A., Shea-Donohue T., Mechanisms of Disease: the role of intestinal barrier function in the pathogenesis of gastrointestinal autoimmune diseases. Nature Clinical Practice